Everyone has a barrier in their brain that’s composed of densely packed cells in the capillary walls, restricting the passage of substances of the wrong size and chemistry from the bloodstream. This blood-brain barrier prevents dangerous intruders from entering, such as infective bacteria.
The down side is that this locked up fence doesn’t defend against just the bad guys, but it also keeps out helpful drugs during an emergency. According to europepmc.org, less than 5% of the roughly 7000 available drugs can pass through, severely limiting the options for new therapies. This is because most drugs are made up of molecules that are too large to get by.
But now there’s hope. Blasts of ultrasound have been used to temporarily open the barrier in certain spots of the brain, and a group of engineers at Chang Gung University in Taiwan have developed a prototype device in a 256-channel ultrasound phased array to improve the delivery of that energy.
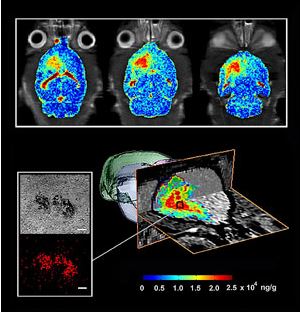
Blasts of ultrasound have been used to temporarily open the barrier in certain spots of the brain. Image: Hao-Li Liu/Chang Gung University
The team developed a unique circuit design involving multiple microcontrollers and power-sensing feedback circuits that allow the system to deliver two frequencies simultaneously instead of the single frequency that biomedical researchers have been testing. By altering the phase of individual channels, the array produces millimeters of wide spots of ultrasound energy that can be electronically steered to any point in the brain.
Although the exact workings haven’t been fully discovered yet, it’s been known for years that ultrasound reversibility opens the blood-brain barrier. According to electrical engineering professor Hao-Li Liu, the process relies on the acoustic cavitation effect, which is the growth and collapse of microbubbles in a liquid under the influence of an ultrasonic field. This effect generates an acoustic shock wave, causing the cells in the blood vessel walls, called endothelial cells, to deform.
After being shocked, endothelial cells contract, generating gaps. Liu said this result increases the possibility of drug delivery without the other cells around the ultrasound’s focal point being disturbed. Doctors would then be able to deliver drugs for about one to two hours, after which the gap closes.
Liu hopes that a clinical trial involving the 256-channel ultrasound system could be launched within three years after gaining the support of neurologists. If and when these capabilities move from the lab to the doctor’s office, better drug therapies will become available.
Story via spectrum.ieee.org.
Advertisement
Learn more about Electronic Products Magazine





