Alternative measures to animal testing took a big step forward recently when the founding director of Harvard’s Wyss Institute, Don Ingber, M.D., Ph.D., received the NC3Rs 3Rs Prize from the U.K.'s National Centre for the Replacement, Refinement and Reduction of Animals in Research (NC3Rs) for his group’s lung-on-a-chip technology — a micro device lined with human cells that replicates the complex functions of an actual living lung.

The Wyss Institute’s award-winning lung-on-a-chip device.
The device offers a new in vitro approach to drug screen testing by mimicking the mechanical and biomechanical behaviors of a human lung. It is expected that this technology will not only decrease animal testing, but also speed up drug development and make medicine more affordable.
“We believe that our human breathing lung-on-a-chip, and other organ chips we have in development, represent a first wave of exciting new alternative approaches to animal testing that hopefully will change how drug development is carried out in the future,” Ingber said. “This award helps to validate this radical new approach on the global stage, and to strengthen our resolve to work with government agencies and pharmaceutical companies that have been supporting our work to pursue this alternative approach to animal testing.”
An inside look at the lung on-a-chip
The device itself is fairly small, about the size of a memory stick or so. It’s made up of a clear, flexible polymer that contains hollow channels fabricated using computer microchip manufacturing techniques.
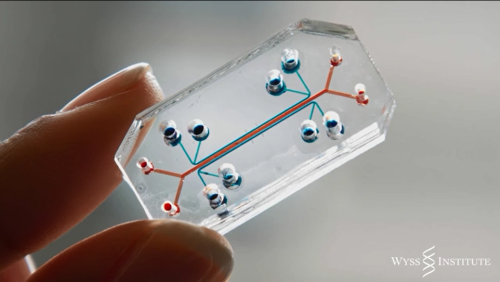
The lung-on-a-chip is about the size of a memory stick.
How the lung-on-a-chip actually works is impressive in its complexity: two of its channels are separated by a thin, flexible, porous membrane. One side is lined with human lung cells from the air sac and exposed to air. On the other side are human capillary blood cells from the lung with medium flowing over their surface to mimic blood flow.
A vacuum is applied to the device’s side channels to deform the tissue-tissue interface, thereby mimicking the way human lung tissues physically expand and retract while breathing.
Testing the lung-on-a-chip
Ingber’s team published a paper in Science Translational Medicine that describes a test they performed in which the lung-on-a-chip was used to mimic pulmonary edema (fluid on the lungs). They introduced the disease to the chip by mimicking a drug toxicity known to produce pulmonary edema in humans, and then studied its progression in real time. Such unprecedented access to information allowed the team to discover several new insights about the condition, including that it’s the physiological breathing motion of the lungs that exacerbates drug toxicity-induced edema.
The following video explores the lung on-a-chip device and the group’s pulmonary edema study:
Outlook
A wide range of “organ chips” have already been produced and tested by Ingber’s team, including devices that can be adjusted to accurately model the lung, heart, liver, kidney, intestine, pancreas, skin, and bone marrow of various animals.
While the breadth and versatility of this technology is impressive, the ultimate goal is to provide drug companies with a system that can simulate numerous organs together, as if they were functioning in a real body.
“My hope is that we can replace one animal model at a time. Probably you’re always going to need animals for certain levels of organ interaction or behavior that you can’t mimic on a chip,” Ingber said. “But in the next five to 10 years we could see a significant reduction in animal testing.”
Story via: wyss.harvard.edu
Advertisement