By Ash Patel & Bahram Mirshab, Healthcare Segment, Renesas Electronics America Inc.
According to the Centers for Disease Control (CDC), approximately 610,000 people die of heart disease in the U.S. every year — that’s one in every four deaths1 . Cardiac health is one of the most important parameters for a person’s overall health. The internet of medical things (IoMT) is enabling a new generation of wearable, multi-parameter, continuous cardiac monitoring systems to improve healthcare management in a variety of hospital, clinic, patient care, and home environments.
The IoMT is a connected infrastructure for medical devices and services that collect and analyze data that is sent to healthcare providers. Today, these devices include sensors that measure temperature, humidity, and vibration, as well as algorithms that identify a limited number of heart conditions.
Next-generation designs are looking to add parameters that would identify a wider range of arrhythmias using smarter and more complex algorithms. For instance, disposable “patches” that resemble invisible bandages with a few, very small ICs could be worn comfortably on the skin for longer times to monitor and manage cardiac health.
Connected cardiac monitoring systems will include three main elements: Wearable wireless sensor node(s), a data management service, and cloud-based analytic platforms.
The electrocardiogram (ECG) sensor node (e.g. ECG patch or heart rate-monitoring conductive garments) and data management service collect cardiac data from the wearable device in a data center. The sensor node is typically a one- or three-lead ECG monitoring device with up to three electrodes (wet or dry) attached to the electronics on the patch.
The cloud-based platform gathers and analyzes the cardiac data using complex algorithms and artificial intelligence (AI) engines to identify potential abnormal heart functionalities. The results can be added to the patient’s medical records and made available to the designated healthcare organization and cardiologist in charge.
Analog front ends
The ECG signal conditioning path (Fig. 1 ) includes the analog stage, which is used to sense, amplify, and cleanup the analog waveform. The ECG signal amplitude ranges from hundreds of microvolts to about 5 millivolts. The signal includes low-frequency (50/60 Hz) noise coupled from AC lines, high-frequency noise from body muscles and often RF noise from different equipment in the proximity of the device. In the case of wearable devices, the ECG signal baseline would have undesirable fluctuation due to motion artifacts.
Thus, highly complex analog front ends (AFE) are often used to clean up and digitize ECG signals. The AFE includes EMI filters to remove RF noise; a high-pass filter with a typical 0.5-Hz corner frequency to remove the base line fluctuation; a low-pass filter with a typical 150-Hz corner frequency to filter out-of-band signal; a notch filter to filter 50/60 Hz noise; a low-noise programable instrumentation amplifier to amplify the signal, and an analog-to-digital converter to digitize the signal for post processing of the sampled data.
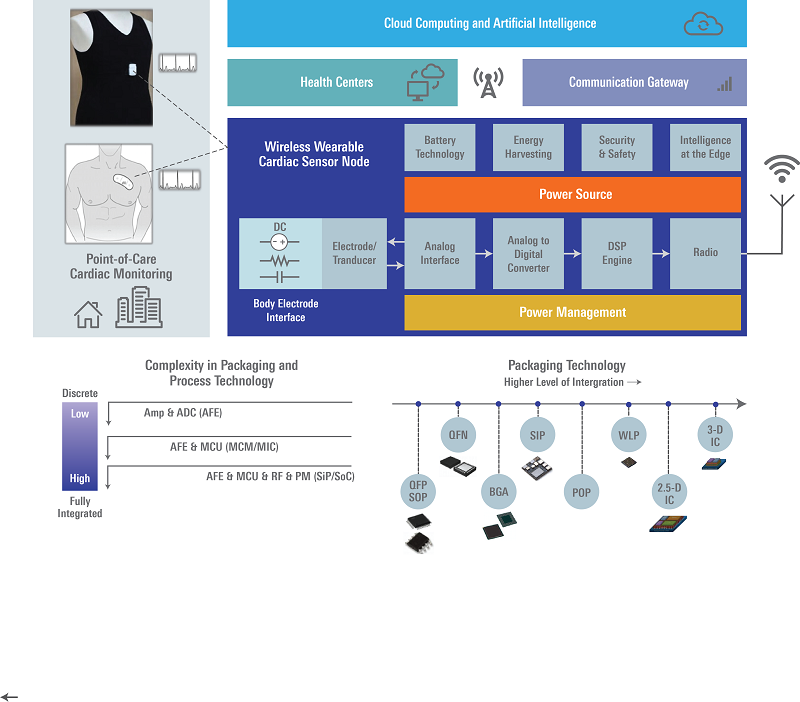
Fig. 1: Typical IoMT connected cardiac monitoring sensor node and the related signal path.
A key requirement for the AFE is to maintain the characteristics of the ECG waveform from the patient throughout the signal path. This is achieved by minimizing the effects of noise and inaccuracies (e.g., gain error, offset error, etc.) throughout the signal path under all operating conditions.
High-performance MCUs
The next stage in the path is a microcontroller (MCU) for post processing and/or housekeeping of the digitized ECG data. Depending on the type of the wearable monitoring device, the sampled raw ECG data in the wearable sensor would be either analyzed on the fly to detect the most common cardiac arrhythmias and then saved in the nonvolatile memory in the system, or stored in the memory for off-line analysis at the end of the device’s lifetime.
The former approach is taken in the newer generation of disposable wearable ECGs, requiring higher-performance MCUs with a DSP engine and higher code/data storage memory to accurately detect several common arrythmias on the fly in addition to storing larger amounts of raw data for post processing. Additional requirements include smaller footprint electronics, precision AFEs and lower power consumption.
The additional memory and higher performance of the MCU introduce challenges in power performance and the size of the die. These challenges need to be addressed by utilizing advanced low-power process nodes with small cell geometry, and by including power management features to allow for efficient power management schemes at the system level.
The system MCU must have low consumption per operating frequency (better than 50 µA/MHz) and include a variety of operating modes with scalable frequency to allow for flexible power management at the system level. A very common method involves cycling of the MCU “on” and “off” with a profile based on some custom proprietary usage models of the system.
As the radio and the MCU dominate power consumption in the system, their usage needs to be as low as possible. To limit power consumption during the power cycling process, the MCU must provide sub-microamp current consumption in standby operation mode and have a very fast transition time (no more than a few microseconds) from standby to the normal operating mode to minimize switching power losses.
The newer AFEs are required to operate continuously at a lower power consumption (typically below 100 µW) and include dedicated low-power digital signal processing circuits (e.g. R-to-R peak period measurement) in addition to the analog signal path. This would lower the amount of signal processing by the MCU. In general, features such as enhanced diagnostics, vital-sign parameter monitoring, and additional signal measurement (e.g. Bio-Z) contribute to the AFE’s complexity.
Ultra-low-power connectivity
The last stage of the signal path in the ECG sensor node is some type of low-power wireless connectivity to enable communication to the gateways such as smartphones or custom sensor hubs. Data transmission to the cloud platform and healthcare centers can include raw ECG data, possible arrhythmia or normal rhythm information as well as some other system parameters measured during the operation. Currently, low-power Bluetooth is one of the most commonly used wireless interface. NB-IoT and CAT-M type of connectivity are being evaluated for future use.
The trend toward smaller form factor, more cost effective, and significantly longer lasting disposable ECG patches means a higher level of integration for the ultra-low-power signal path in a tiny system on chip (SoC) or system in package (SIP) device. Some challenges faced in the miniaturization of the electronics are the need for a cost-effective semiconductor process node suitable for low-power precision mixed-signal (analog and digital) circuitries, and the availability of a more cost-effective small footprint packaging technology.
Ultra-low-power consumption is one of the key requirements for this new type of ECG patch, as it can significantly increase the continuous cardiac signal monitoring/analysis lifetime beyond the current duration of seven to 15 days. Lower power consumption also allows developers to include additional vital sign monitoring, which gives them a competitive advantage.
Currently, patches use single-coin type batteries with a typical capacity of several hundred mAh. However, there are efforts to use smaller, lower capacity and more cost-effective batteries combined with an energy harvesting method using “battery-less” sensor nodes based on specialized new semiconductor process technologies such as silicon-on-thin-buried-oxide (SOTB) and sub-threshold processes.
The challenge of transitioning energy harvesting-based cardiac monitoring patches from research labs to the market is the availability of continuous and consistent energy sources to harvest at the point of use. The industry is exploring the use of sources such as body heat, vibration from motion, or dedicated RF energy in the surrounding environment to address this key challenge.
Finally, cardiac monitoring SoC design would require successfully integrating mixed mode circuits on a very small piece of silicon without interference across the allocated boundaries in the layout. This would require special design expertise to prevent the propagation of noise generated by high-frequency switching digital and RF circuits to the neighboring precision analog circuity.
The IoMT is shifting traditional reactive healthcare towards a more affordable preventive system with potentially lower costs. Combining advancements in semiconductor, connectivity, and material science technologies with the power of AI offers the potential for life-altering applications for the betterment of society.
Advertisement
Learn more about Electronic Products MagazineRenesas Electronics America





